What is Erysipelas ?
It is a skin disease which features acute bacterial infection of the shallow lymphatic tissues and the outer dermis.It means that the upper or superficial layers of the skin get infected by bacteria. The most common pathogen is group A streptococcal bacteria, particularly streptococcuspyogenes.
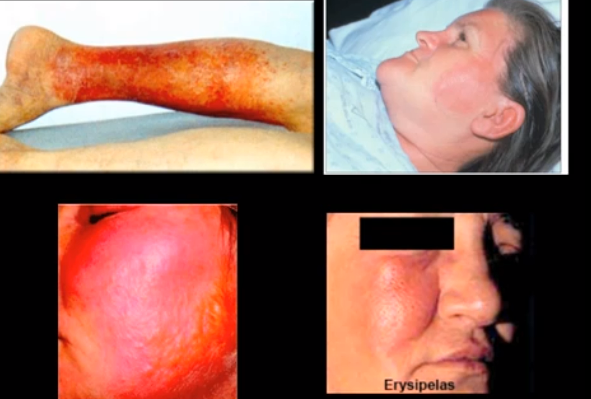
Erysipelas leads to formation of a striking red rash with elevated borders. It can be easily differentiated from the adjacent skin. The infected skin may be warm to touch. In the past, it was commonly believed that erysipelas usually affected the face. However, current studies have indicated that the skin inflammation is distributed across the body, and the legs get affected in nearly 80 percent of patients. The rash can also occur on the trunk and arms.
Erysipelas usually starts after a mild trauma like a burn, bruise, incision, or wound. The occurrence of rash on the legs, torso, or arms is generally at the location of a wound or a surgical incision.In some countries, erysipelas is also known by varied names like ‘Ignis sacer’, ‘holy fire’,or ‘St. Anthony’s fire.’
Erysipelas Symptoms
The signs and symptoms of erysipelas are listed below:
- An inflamed, thick, warm, and bright red rash appears on the affected skin. It has features similar to an orange peel.
- The rash may be very painful
- The erythematous skin lesion may quickly enlarge and elicit a clear and raised edge or border.
- Severe infections can result in the development of vesicles, bullae, and petchaie, along with minor signs of skin necrosis or death of skin.
- There may be swelling of the lymph nodes resulting in lymphedema. In some patients, doctors may also observe the occurrence of a reddish strip that stretches to the lymph node.
- Patients may also experience a variety of symptoms such as shaking, high fever, tremors, chills, exhaustion or weakness, headaches, vomiting, minor illness or malaise in a 48-hour period that follows the initial infection.
- Erysipelas may affect the skin occurring in any part of the body. The infection may occur on the legs, arms, fingers, face, toes, and the trunk. The disease is however more prevalent at the extremities. Fat tissue is most prone to developing the erysipelas infection. Facial areas near the eyes, ears, cheeks, and nose are also equally vulnerable.
Erysipelas may cause a number of health complications, some of which are as follows:
- Migration of the infection to different sections of the body through the bloodstream, which can result in septic arthritis, and/or infective endocarditis which affects the heart valves.
- A deadly effect called septic shock
- Reappearance of the erysipelas bacterial infection. As per available statistical data, the disease tends to recur in about 18 to 30 percent of patients, even after successful antibiotic treatments.
- Lymphatic system damage
- An erysipelas infection can deteriorate to a very dangerous condition called necrotizing fasciitis, when the infection spreads to tissues occurring deeper within the body.
- Persistent and recurring infection of the limbs can lead to chronic inflammatory conditions like lymphadenitis.
Causes of erysipelas
- Most instances of erysipelas are caused by Streptococcus pyogenes bacterial infection. The bacteria are also called beta-hemolytic group A streptococci.
- Erysipelas may also be caused due to infection by non-group A streptococci bacteria. GBS, or group B strep, or Streptococcus agalactiae bacteria are a part of beta-hemolytic non-group A streptococci family.
- The characteristic erysipelas rash is caused by an exotoxin, and not only by the bacterium. The infection usually occurs in areas where no symptoms are visible. For example, the naso-pharynx area may be affected by the infection, but the rash may appear on the face or the arms.
- The bacteria may enter the skin through various means such as minor cuts or injuries, insect bites, dog bites, eczema, surgical cuts, and ulcers. Most infections originate from the strep bacteria that are present in the nasal passages of the patients.
- The infection tends to set in after the deterioration and growth of a tiny scratch or bruise, eventually resulting in toxaemia
- Erysipelas typically affects infants, children, and the elderly. People with compromised immune systems, deficient lymphatic clearance, and conditions like diabetes, skin ulcers, alcoholism, and fungal infections are also at elevated risk to developing erysipelas. The resultant infection does not affect the subcutaneous tissue. It does not result in discharge of pus, but only serum or serous fluids.
Erysipelas vs Cellulitis – The Difference
The presence of subcutaneous edema may make the doctor misdiagnose the disease as cellulitis. It may however be noted that the structure of an erysipelas rash is more compact with demarcated edges as opposed to a cellulitis rash.
In the past, it was widely believed that only the face was subject to erysipelas infections. It has now been determined that the disease is most prominent on the legs.
Diagnosis of erysipelas
- Erysipelas is mainly diagnosed via the appearance of the distinctive rash and the presence of inflammation.
- It is possible to visually distinguish erysipelas from cellulitis via the well-defined, sharp, and raised borders of the rash. Doctors will also notice the rise of ASO or antistreptolysin O titer, about 10 days after initial infection.
- Blood cultures do not help in correct diagnosis. It can however be used to confirm sepsis. It is also essential to differentiate erysipelas from other disorders like herpes zoster, angioedema, contact dermatitis, and diffuse inflammatory carcinoma of the breast.
Treatment of erysipelas
- Treatment of erysipelas is dependent on the severity of the condition. Penicillin is the preferred antibiotic as the bacteria are sensitive to it. The antibiotic may be given intravenously or orally. People who are allergic to penicillin may be treated with erythromycin.
- The treatment lasts for 10 to 14 days. The symptoms of general illness usually alleviate within 1 to 2 days. However, the skin abnormalities may completely recover only after some weeks. Scarring does not occur.
- Erysipelas causes lymphatic damage which results in lowered toxin removal from the body. This is the reason why erysipelas patients are at increased risk to reoccurrence of infection. Some doctors may suggest use of prophylactic antibiotics after treatment to prevent a relapse. This however does not guarantee prevention of reoccurrence.
Erysipelas Pictures



There are some attention-grabbing time limits in this article but I dont know if I see all of them middle to heart. There is some validity however I’ll take hold opinion till I look into it further. Good article , thanks and we would like extra! Added to FeedBurner as nicely
Thanks for the beneficial post. Expect to see much more in the near future.
This post has been extremely helpful to me. Thank you.